Biomarkers. Sounds important. What are they? What can they really tell us?
 Researchers
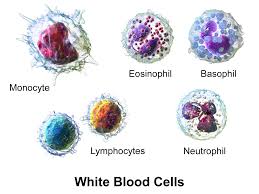
have been seeking to find a connection between nonspecific biomarkers
(things we ALL have circulating in our blood) like LDH, various white
blood cells (neutrophils and monocytes - whether as an absolute count or
as a neutrophil to lymphocyte ratio), myeloid-derived suppressor cells
(MDSCs) and T-regs (See post with links about all that here: Blood markers associated with clinical outcomes). And
while many meaningful correlations have been drawn between these
components and response to treatment (or lack thereof); the fact that
they are all affected by numerous circumstances other than melanoma and
its treatment, create limitations in the clarity with which they can be
used to PREDICT responses.
Researchers
have been seeking to find a connection between nonspecific biomarkers
(things we ALL have circulating in our blood) like LDH, various white
blood cells (neutrophils and monocytes - whether as an absolute count or
as a neutrophil to lymphocyte ratio), myeloid-derived suppressor cells
(MDSCs) and T-regs (See post with links about all that here: Blood markers associated with clinical outcomes). And
while many meaningful correlations have been drawn between these
components and response to treatment (or lack thereof); the fact that
they are all affected by numerous circumstances other than melanoma and
its treatment, create limitations in the clarity with which they can be
used to PREDICT responses.
With recent scientific advances, PCR testing (Polymerase chain reaction) has become more efficient and cost-effective, allowing labs to copy or "amplify" small segments of DNA or RNA though screening blood or other biological specimens. This ability allows the cellular identification of whatever may be floating in that blood sample....whether it is a virus or fungus, or actual bits and pieces of tumor cells themselves, to allow a determination of disease burden, prognosis, and response to treatment. Here is an earlier post: Circulating tumor cells: how they may eventually impact melanoma diagnosis and evaluation of response
Now there are these reports:
Liquid biopsy utility for the surveillance of cutaneous malignant melanoma patients. Haung and Hoon. Mol Oncol. 2015 Dec 17.
Circulating melanoma cells as a potential biomarker to detect metastasis and evaluate prognosis. Hida, Yoneta, Wakamatsu, et al. Australas J Dermatol. 2016 Mar 1.
With recent scientific advances, PCR testing (Polymerase chain reaction) has become more efficient and cost-effective, allowing labs to copy or "amplify" small segments of DNA or RNA though screening blood or other biological specimens. This ability allows the cellular identification of whatever may be floating in that blood sample....whether it is a virus or fungus, or actual bits and pieces of tumor cells themselves, to allow a determination of disease burden, prognosis, and response to treatment. Here is an earlier post: Circulating tumor cells: how they may eventually impact melanoma diagnosis and evaluation of response
Now there are these reports:
Liquid biopsy utility for the surveillance of cutaneous malignant melanoma patients. Haung and Hoon. Mol Oncol. 2015 Dec 17.
Cutaneous
melanoma is one of the highest incident-rate cancers with increasing
prevalence in Western societies. Despite the advent of new approved
therapeutics, the 5-year overall survival rate of stage IV melanoma
patients remains below 15%. Current treatments for late stage disease
have shown higher efficacy when treated at a lower disease burden. Thus,
blood-based biomarkers capable of detecting melanoma prior to
clinically evident distant metastasis, will improve the treatment and
outcomes for melanoma patients. To that end, effective treatment of
melanoma necessitates identification of patients at risk for developing
distant metastases. Furthermore, employing blood biomarkers that monitor
cancer progression over the course of treatment is a promising solution
to post-treatment drug resistance often developed in melanoma patients.
Non-invasive blood biomarker assays allow for regular dynamic
monitoring of disease. "Liquid Biopsy" of blood, which exploits
circulating tumor cells (CTCs), cell-free circulating tumor DNA (ctDNA)
and cell-free circulating microRNA (cmiRNA), has been shown to detect
prognostic factors for relapse in AJCC stage III and stage IV melanoma
patients. Moreover, molecular characterization of CTC and analysis of
various forms of ctDNA present promising potential in development of
individualized therapy for melanoma patients. New approaches such as
massive parallel sequencing (MPS) provide a comprehensive view of the
disease progression, allowing for the selection of therapeutic options
for individual patients. With advancements of improving molecular
assays, liquid biopsy analysis as a powerful, routine clinical assay for
melanoma patients, is highly promising prospective.
|
Circulating melanoma cells as a potential biomarker to detect metastasis and evaluate prognosis. Hida, Yoneta, Wakamatsu, et al. Australas J Dermatol. 2016 Mar 1.
Then, there's the examination of the properties of the tumor sample itself. This article talks about looking at the tumor in regard to how well it is being recognized by the immune system....specifically t-cells:
Melanoma-specific MHC-II expression represents a
tumour-autonomous phenotype and predicts response to anti-PD-1/PD-L1 therapy. Johnson, Estrada, Salgado, Sosman, et al. Nat Commun.
2016 Jan 29.
Here...the tumor is being characterized by surface molecules that are correlated with prognosis:
Molecular markers to complement sentinel node status
in predicting survival in patients with high risk locally invasive melanoma. Rowe, Tang, Hughes, et al. Int J Cancer. 2016 Mar 14.
Here the tumor is being analyzed for specific genetic variations:
Genomic and Transcriptomic Features of Response to
Anti-PD-1 Therapy in Metastatic Melanoma. Hugo, Zaretsky, Sun, et al.
Cell. 2016 Mar 15.
PD-1 immune checkpoint
blockade provides significant clinical benefits for melanoma patients. We
analyzed the somatic mutanomes and transcriptomes of pretreatment melanoma
biopsies to identify factors that may influence innate sensitivity or
resistance to anti-PD-1 therapy. We find that overall high mutational loads
associate with improved survival, and tumors from responding patients are
enriched for mutations in the DNA repair gene BRCA2. Innately resistant tumors
display a transcriptional signature (referred to as the IPRES, or innate
anti-PD-1 resistance), indicating concurrent up-expression of genes involved in
the regulation of mesenchymal transition, cell adhesion, extracellular matrix
remodeling, angiogenesis, and wound healing. Notably, mitogen-activated protein
kinase (MAPK)-targeted therapy (MAPK inhibitor) induces similar signatures in
melanoma, suggesting that a non-genomic form of MAPK inhibitor resistance
mediates cross-resistance to anti-PD-1 therapy. Validation of the IPRES in
other independent tumor cohorts defines a transcriptomic subset across distinct
types of advanced cancer. These findings suggest that attenuating the
biological processes that underlie IPRES may improve anti-PD-1 response in
melanoma and other cancer types.
While none of these (other than those that are simple measures of recognized blood components) are validated and ready for daily screening of cancer patients across this country....every step is important in helping docs...eventually....determine
the best treatment options for the individual and monitor their
response to that treatment in ways that are specific, easily measured,
and less invasive and damaging to that patient. What a beautiful day that will be!!! Minimized only by the day we figure out how to avoid cancer entirely! Hey....might as well live large and dream big!!! - c
No comments:
Post a Comment